Agentic AI Reshapes Healthcare Revenue Cycle Management Systems
More and more healthcare systems are using agentic AI to automate patient interactions and administrative tasks. According to McKinsey, providers could save between $60 million and $120 million each year. The technology also makes it possible for large healthcare networks to make up to $6 billion more in revenue.
Agentic AI tools take care of scheduling, billing, coding, claims processing, and checking insurance automatically. This makes complex revenue cycle operations more accurate while cutting down on manual work. Providers get better financial stability while still focusing on the quality of clinical service delivery.
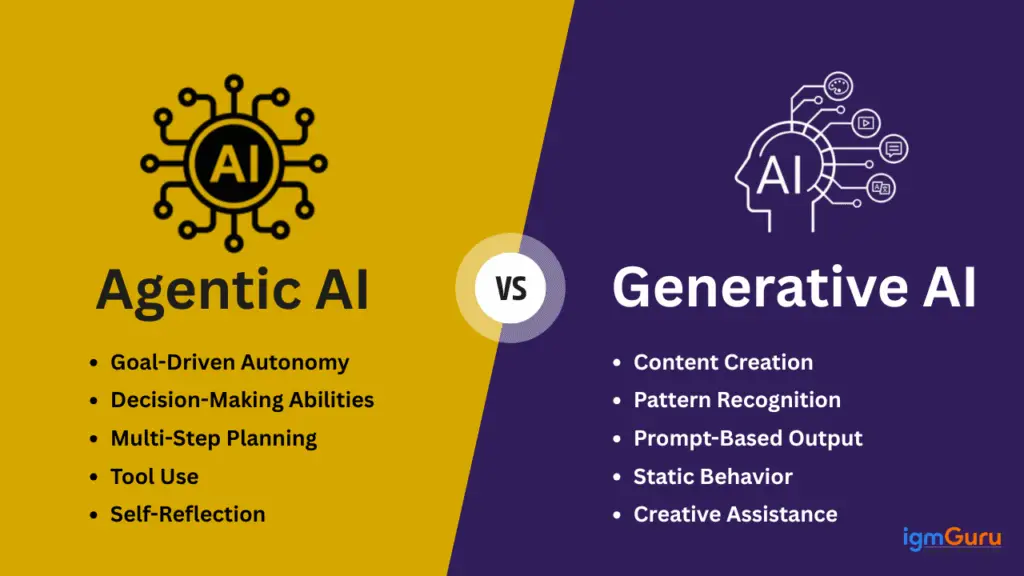
Source: igmGuru
Automation Cuts Collection Costs and Accelerates Cash Realization Timelines
According to a McKinsey study, AI could cut the cost of collecting money by 30% to 60%. Automated workflows get rid of repetitive tasks that used to need a lot of administrative staff to do. Faster processing means faster reimbursement cycles and better management of an organization’s cash flow.
AI help has made it easier for healthcare finance teams to get payments on time and have fewer claims denied. Agentic systems keep an eye on the progress of claims all the time and fix mistakes in documents on their own. This makes it easier to predict cash flow for all hospitals and outpatient service providers across the country.
Providers Increasingly Prioritize AI Deployment Across Revenue Workflows
Over 30% of providers put AI and automation projects at the top of their lists in 2025. This was an increase from 4 to 5 use cases that were used in 2023 and 2024. Organizations can now deploy across 7 major revenue cycle management functions at the same time.
Hospital leaders think that using AI is necessary to stay competitive in business. The growing need for workers and pressure to pay for them faster are making people more interested in intelligent automation platforms. More and more strategic investment decisions favor technology-driven solutions for optimizing revenue.
Recommended Article: Trump Imposes 25% Tariff on Selected AI Chip Imports
Prior Authorization Leads Demand for Front End AI Solutions
During 2025, RCM leaders were most interested in AI-powered prior authorization solutions. About 60% put automation at the top of their list when it came to patient access and eligibility verification. This shows that there are still administrative problems that are slowing down care delivery and payment for providers.
Only 44% of people who planned to use AI in 2024 said they would do so within 3 years. The rise in demand shows how frustrated people are getting with delays in getting insurance approval. Automated prior authorization cuts down on the time patients have to wait and lowers the chances of claims being denied.
Documentation Improvement Drives Middle Cycle AI Adoption Growth
During 2025, clinical documentation improvement tools were in the highest demand in the middle of the cycle. Adoption went up significantly from the previous year’s 20%. Accurate clinical documentation helps with billing and reimbursement strategies that follow the rules and get the most money.
AI systems help doctors by automatically organizing notes and making coding suggestions. This makes it easier to write down information and makes coding more accurate. Better data quality makes it easier to get ready for an audit and negotiate with payers.
Denials and Appeals Dominate Backend AI Implementation Priorities
61% of demand for backend processes was for automating claim denials and appeals. Only 23% planned to do this in the past year. The increasing complexity of claims makes it necessary to have smart tools for resolving disputes quickly.
Agentic AI looks at patterns of rejection and automatically makes appeal documents for providers. This makes it more likely that people will get their money back for reimbursements that were lost or delayed. Automation cuts down on lost revenue that happens because of mistakes made by administrators or inconsistencies in paperwork.
Patients Gain Faster Access and Simplified Billing Experiences
McKinsey said that patients benefit from faster approvals for treatment and clearer bills. Less friction in the office means shorter wait times between diagnosis and scheduling therapeutic intervention. Patients are much happier and more trusting of healthcare providers when billing is clear.
Providers can move staff around to work on activities that get patients involved when revenue workflows are streamlined. Improving administrative efficiency directly helps with coordinating care and personalizing services. Agentic AI thus enhances both financial viability and the overall quality of the healthcare experience.